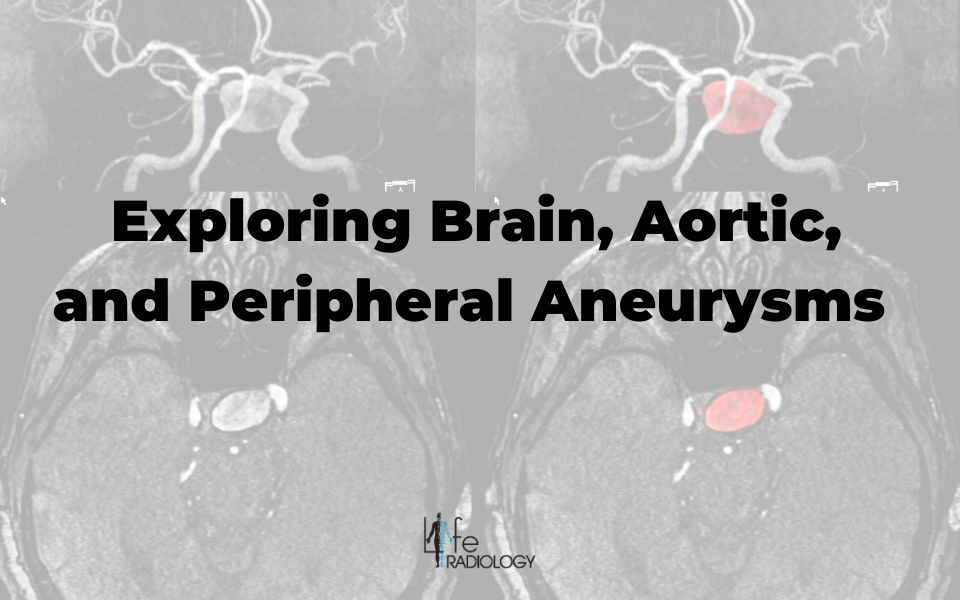
Exploring Brain, Aortic, and Peripheral Aneurysms
An aneurysm is not merely a medical term; it is a time bomb within the walls of your arteries. Aneurysms, which often lurk silently, exhibit a bulge or dilation in the artery wall, typically originating from a weak area in the arterial structure. Left untreated, aneurysms possess the potential to burst open, resulting in life-threatening internal bleeding.
Equally perilous, they can trigger the formation of blood clots that obstruct the natural flow of blood within the artery. The location of aneurysms significantly influences their potential dire consequences, as a rupture or clot can rapidly escalate into a life-threatening scenario.
In this comprehensive guide, we will delve into the various types of aneurysms, their causes, symptoms, risk factors, diagnosis, and treatment options, unraveling the enigmatic world of these arterial time bombs.
What is an Aneurysm?
Is a medical condition characterized by a localized, abnormal dilation or ballooning of a blood vessel, typically an artery, which poses a significant risk of rupture and potentially life-threatening consequences.
What Are Different Types of Aneurysms?
Aneurysms occur in various artery locations in the body, including the heart, abdomen, brain, and legs. The specific location determines the type of aneurysm. The most common type is the aortic aneurysm, which forms in the aorta, the largest artery carrying blood from the heart. Aneurysms that develop in arteries other than the aorta are called peripheral aneurysms.
Cerebral Aneurysms: Silent Threats in the Brain
Cerebral aneurysms, also known as intracranial or brain aneurysms, occur within the blood vessels of the brain, particularly at the branching points of arteries.
Symptoms of Cerebral Aneurysms:
- Sudden and Severe Headache: Often described as the worst headache of one's life, this headache can come on suddenly and be unbearable.
- Vision Problems: Visual disturbances, such as double vision, blurred vision, or light sensitivity.
- Nausea and Vomiting: Nausea and vomiting may occur in conjunction with the headache.
- Neck Pain or Stiffness: Some individuals experience neck pain or stiffness.
- Seizures: In some cases, a ruptured cerebral aneurysm can trigger seizures.
- Altered Mental State: Confusion, drowsiness, or loss of consciousness.
Risk Factors for Cerebral Aneurysms:
- Family History: A family history of aneurysms can increase the risk, suggesting a genetic predisposition.
- High Blood Pressure: Hypertension places chronic stress on blood vessel walls, making them more susceptible to aneurysm formation.
- Smoking: Smoking is a significant contributor to the development and rupture of cerebral aneurysms.
- Certain Medical Conditions: Conditions like polycystic kidney disease and connective tissue disorders can elevate the risk.
Causes of Cerebral Aneurysms:
- Weak Blood Vessel Walls: Weakness in the arterial wall can make it prone to bulging and aneurysm development.
- Hemodynamic Stress: Blood flow patterns and forces within the arteries may play a role in aneurysm formation.
- Atherosclerosis: The buildup of fatty deposits in the arteries can contribute to aneurysm development.
Diagnosis of Cerebral Aneurysms:
- Imaging Tests: Magnetic resonance angiography (MRA) and computed tomography angiography (CTA) provide detailed images of the blood vessels, allowing for the identification of cerebral aneurysms.
- Cerebral Angiography: This invasive procedure involves the injection of a contrast dye into the blood vessels to visualize the aneurysm with high precision.
- CT or MRI scans: These imaging techniques can also help detect and assess cerebral aneurysms.
Treatment for Cerebral Aneurysms:
- Surgical Clipping: A neurosurgeon places a metal clip at the neck of the aneurysm to prevent it from rupturing.
- Endovascular Coiling: This minimally invasive procedure involves inserting coils into the aneurysm to block blood flow and promote clotting within the aneurysm sac.
- Flow Diversion: A stent-like device, known as a flow diverter, can divert blood flow away from the aneurysm when placed across it.
- Observing: Smaller aneurysms or those in locations less prone to rupture may undergo ongoing monitoring without immediate intervention.
Aortic Aneurysms: The Silent Dilations of the Body's Lifeline
Aortic aneurysms develop in the aorta, the body's largest artery. They can occur in two primary locations: the thoracic aorta (in the chest) and the abdominal aorta (in the abdomen).
Symptoms of Aortic Aneurysms
- Pain: Some people may feel localized pain or discomfort in the chest or abdomen.
- Back Pain: Back pain is a common symptom, especially in the case of thoracic aortic aneurysms.
- Pulsatile Mass: Feeling a pulsating mass in the abdomen may indicate an abdominal aortic aneurysm
- Other Symptoms: Nonspecific symptoms such as fatigue, loss of appetite, or weight loss may also be present.
Risk Factors for Aortic Aneurysms:
- Age: Aortic aneurysms are more common as individuals age, especially in those over 60.
- Gender: Men are more likely than women to develop aortic aneurysms.
- Family History: A family history of aortic aneurysms can elevate the risk.
- High Blood Pressure: Hypertension can weaken the aorta's walls.
- Smoking: Smoking is a significant risk factor for aortic aneurysm development and rupture.
- Atherosclerosis: The presence of atherosclerosis, or the buildup of plaque in the arteries, can increase the risk.
Causes of Aortic Aneurysms:
- Degenerative Changes: Gradual wear and tear on the aortic walls over time can lead to aneurysm formation.
- Inflammatory Conditions: Infections or autoimmune diseases can lead to aortic inflammation, weakening the vessel walls.
- Genetic Factors: Some individuals may have a genetic predisposition to develop aortic aneurysms.
Diagnosis of Aortic Aneurysms:
- Imaging Tests: Ultrasound, computed tomography angiography (CTA), and magnetic resonance angiography (MRA) provide detailed images of the aorta, allowing for aneurysm detection and evaluation.
- Chest or Abdominal X-rays: These may reveal an enlarged aorta.
- Echocardiography: This ultrasound imaging method examines the heart and aorta.
Treatment for Aortic Aneurysms:
- Surgical Repair: Open surgical repair involves replacing or repairing the weakened portion of the aorta with a graft.
- Endovascular Stent Grafting: In this minimally invasive procedure, a stent graft is inserted into the aneurysm to divert blood flow and prevent rupture.
- Medication: Doctors may prescribe blood pressure management and medications to reduce the risk of aneurysm growth.
- Lifestyle Changes: Quitting smoking, managing blood pressure, and maintaining a heart-healthy diet and exercise routine are crucial.
Peripheral Aneurysms: A Hidden Threat in the Extremities
Peripheral aneurysms develop in blood vessels outside the brain and aorta, typically in the arms and legs.
Symptoms of Peripheral Aneurysms:
- Pain: Localized pain at the site of the aneurysm, which can range from mild discomfort to severe, throbbing pain.
- Swelling: The aneurysm may cause swelling, often accompanied by tenderness.
- Pulsating Mass: A palpable pulsating mass or lump at the site of the aneurysm is a common sign.
- Limb Discoloration: In some cases, there may be changes in skin color, such as bluish or reddish discoloration, near the aneurysm.
- Reduced Blood Flow: A peripheral aneurysm can impede blood flow in the affected artery, leading to coldness and numbness in the limb.
- Ulceration and Tissue Damage: Severe cases of peripheral aneurysms can result in tissue damage, skin ulcers, or even gangrene in the affected limb.
Risk Factors for Peripheral Aneurysms:
- Atherosclerosis: Atherosclerosis is a major risk factor, as it can weaken arterial walls, making them more prone to aneurysm formation.
- Trauma: Injuries to blood vessels, particularly in the extremities, can lead to the development of aneurysms.
- Infection: Although less common, infections in the blood vessels can also cause aneurysms.
Diagnosis of Peripheral Aneurysms:
- Physical Examination: A physician may identify a pulsating mass or other physical signs.
- Ultrasound: Ultrasound imaging is a common tool for detecting and assessing peripheral aneurysms.
- CT Angiography (CTA) or Magnetic Resonance Angiography (MRA): These imaging techniques provide detailed images of the affected blood vessels.
- Digital Subtraction Angiography (DSA): In this invasive procedure, healthcare providers inject contrast dye into the blood vessels to visualize the aneurysm.
Treatment for Peripheral Aneurysms:
- Surgical Repair: Open surgical repair involves removing or replacing the weakened portion of the artery with a graft.
- Endovascular Procedures: Minimally invasive techniques, such as endovascular stent graft placement, may be used to exclude the aneurysm from blood flow.
- Observing: Healthcare providers may closely monitor small and asymptomatic aneurysms without immediate intervention.
- Medication: Healthcare providers may prescribe medication in some cases to control blood pressure and reduce the risk of further aneurysm growth.
Vital Detection: Medical Screening and MRI for Early Detection of Aneurysms
Early aneurysm screening at Life Radiology is vital for timely detection and management. Aneurysms are often symptomless until they become critical, and ruptures can lead to life-threatening emergencies. Medical screening and MRI at Life Radiology enable early detection and interventions, potentially saving lives and improving patient outcomes.
In conclusion, understanding the types, causes, and diagnostic methods for aneurysms is essential. If you have concerns about an aneurysm, consult a healthcare professional and follow preventive measures to ensure your well-being. Early detection and proper management can save lives and prevent complications associated with aneurysms.
FAQs
How can I find out if I have an aneurysm?
If you suspect you may have an aneurysm or have risk factors, consult a healthcare professional. Diagnostic tests, including various imaging techniques, can help identify aneurysms.
How can I prevent and manage an aneurysm?
- Lifestyle changes: Quit smoking, manage blood pressure, and maintain a healthy diet and weight.
- Regular check-ups: Routine medical check-ups can detect risk factors.
- Medication: If you have underlying conditions like high blood pressure, follow your doctor's advice.
- Surgical intervention: Depending on the size and location, aneurysms may require surgical treatment to prevent rupture.
What should I do if I suspect I have an aneurysm or experience symptoms?
Seek immediate medical attention if you suspect an aneurysm or experience severe headaches, pain, or other symptoms. Early diagnosis is crucial for timely treatment.
Are there any complications associated with aneurysms?
Yes, untreated aneurysms can rupture, causing severe internal bleeding, which can be life-threatening. Aneurysms can also lead to blood clots, potentially blocking blood flow in arteries.
Is there a genetic component to aneurysms?
Yes, a family history of aneurysms can increase an individual's risk, indicating a genetic predisposition in some cases.